Total Hip Replacement
Patient Information
Total Hip Replacement (THR) is a successful operation performed for pain relief and improved function of those suffering from advanced arthritis of the hip joint. In scientific literature, THR is usually referred to as Total Hip Arthroplasty.
The most common reason for THR in Australia is osteoarthritis, which wear and tear of cartilage. However, a THR may be performed for other conditions such as rheumatoid arthritis, avascular necrosis, and traumatic neck of femur fractures. Arthritis in the hip joint may cause pain and stiffness severely affecting your quality of life. You may need surgery if medication and other forms of non-operative management have failed to control your pain. During your appointment, you will have a thorough assessment and discussion whether you are suitable for total hip replacement.
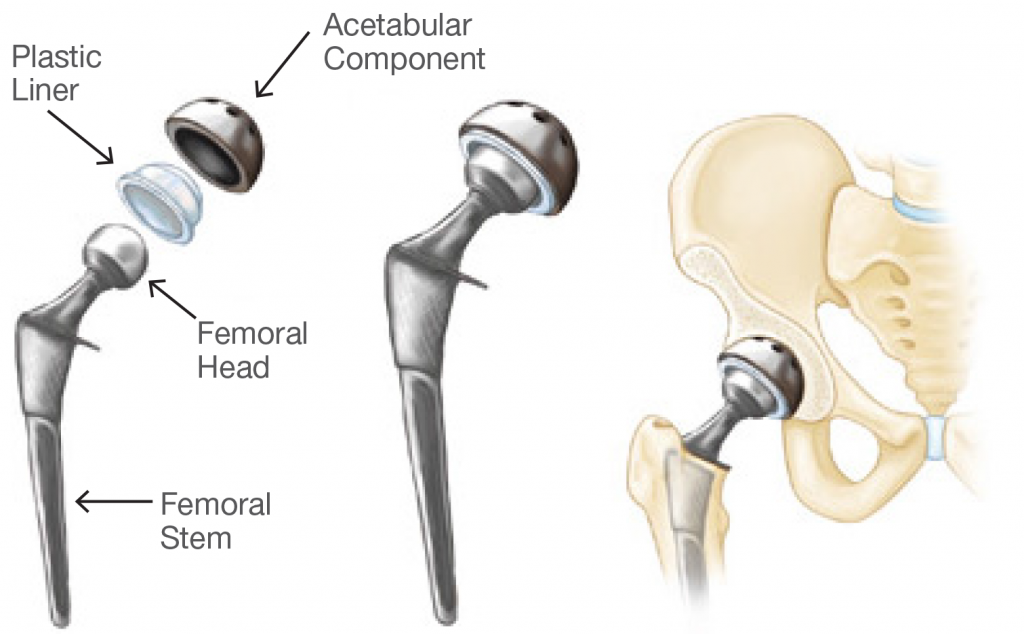
Total Hip Replacement surgery involves removing the damaged bone and cartilage and replacing the joint with artificial implants in order to reduce pain and restore function of the hip joint. The cup (acetabular component) is usually made from titinium and sticks to the native bone. The femoral component is either made from titanium or stainless steel which anchored into the femur using a specialized form of cement. A durable and specialized form of plastic called Polyethylene or ceramic bearing surface is placed between the two metal surfaces in order to allow natural movement of the hip joint with minimal friction.
Multiple successful approaches have been utilized to perform a THR. The two most common approaches are Anterior and Posterior Approaches. Mr. Solaiman offers both techniques for patients who are suitable for surgery. Please discuss your options during your appointment.
Before The Procedure
You may be referred to a physician for preoperative assessment of fitness for surgery and optimization of your health prior to surgery. The physician will also review you on a regular basis post surgery to ensure that you are recovering well from surgery and minimize medical complications.
You will also be referred to a Pre Admission Clinic where you will be assessed by a qualified nurse. Some tests such as ECG, bloods, urine test, and other tests may be ordered during this visit in order to ensure you are fit for surgery. You will also be given a cholorohexidine solution to wash your body prior to surgery.
Fasting
Please ensure that you do not eat or drink for at least for 6 hours prior to surgery. If your surgery is in the morning, you should fast from midnight the night before surgery. However, you can take your usual medications (such as Blood Pressure Medications) with sips of water in the morning. If your surgery is in the afternoon, you can have an early light breakfast and fast from 7 am. Please ask the nurse at pre admission clinic, your anaesthetist, or your surgeon if you have any further questions.
Type of Anaesthetic
Hip replacement surgery requires anesthesia. Your input and preference help the anaesthetic team decide whether to use general anesthesia, which makes you unconscious, or spinal anesthesia, which leaves you awake but unable to feel pain from your waist down. You can discuss these options with your anaesthetist.
You’ll be given an intravenous antibiotic before, during and after the procedure to help prevent post-surgical infection. Unless contraindicated you will also be given tranexamic acid, which reduces your risk of intraoperative bleeding and need for blood transfusion. Local anaesthetic is injected around the hip joint at the end of surgery in order to minimize your post- operative pain.
After The Procedure
You’ll be taken to a recovery room where you will be monitored for 30 min to an hour. You’ll then be moved to your room in the orthopaedic ward, where you’ll likely stay for 3-4 days. Oral medications prescribed by your doctor should help control pain.
You will commence walking either same day or the following day after surgery with the help of a physiotherapist. You’ll also be asked to do frequent breathing exercises and gradually increase your activity level. Your progress during your stay will help determine whether you are suitable for inpatient rehabilitation or discharge home. Your physical therapy will continue following your discharge as outpatients. Upon discharge, you will be sent home with oral analgesia. Please take them as instructed by your doctor.
Wound Care /
Sutures / Dressings
Mr. Solaiman uses absorbable sutures except in rare cases. There will be no need for removal of sutures. You can commence having a shower the day following surgery without worrying about the wound getting wet. The plastic dressing is waterproof. It may be exchanged by nursing staff if it becomes wet.
The dressing can be removed at 12 to 14 days post surgery. If you are discharged home from the hospital, your dressing will be removed and wound checked at your next appointment with Mr. Solaiman usually about 2 weeks from date of surgery. However, if you are transferred to a Rehab Facility and remain there for at least two weeks, your dressing will be removed by rehab nursing staff. You can contact Mr Solaiman’s office if you have any concerns.
Please note: It is important to keep your dressing dry at all times.
Follow Up Appointment
An appointment will be made for you to see Mr Solaiman in the rooms at two weeks if you are discharged home. If you are transferred to a rehab facility, you will be given an appointment at 6 weeks.
Results
Total Hip Replacement provides pain relief, improved mobility and a better quality of life. Most THR can be expected to last more than 15 years. The average rate of revision for a THR in Australia at 15 years is about 8 percent.

Risks
Although THR is a successful surgery, it does carry some risks including but not limited to infection, bleeding, blood clot, dislocation, leg length discrepancy.
Individual patient’s risk profile varies based on their age and medical history. A history of previous blood clots increases the risk of blood clot while diabetes increases the risk of infection compared to normal population. Your risk will be assessed by your surgeon and managed accordingly. Every effort will be made by the treating team to minimize your risks such as antibiotics during and after surgery, blood thinners for 4 to six weeks and calf/foot pump in the hospital. If you have any concerns regarding any specific risks, please discuss it with your surgeon.
DVT Prevention
The risk of symptomatic DVT and Pulmonary Embolism (blood clot in the lung) is less than 1% following total joint replacement surgery. Studies have shown that a combination of three modalities that reduce the risk of DVT/PE include:
- Early Mobilization
- Foot Pump or Calf Compressors
- Blood thinners
You will be given a blood thinner in addition to a mechanical device such as foot pump following surgery. You will also be encouraged to mobilize with the help of our physiotherapist as soon as possible
Return to Work/Activities
You can return to most low demand activities such as office duties about 4-6 weeks post surgery. If you have a physically demanding job such a climbing ladders and driving trucks, you may need longer time. You are encouraged to avoid high impact activities such as running and jumping off the back of a truck. However, you are encouraged to maintain low impact exercises such as cycling, swimming and walking. You can commence driving approximately 4 to 6 weeks post surgery when you
- Have no pain
- Are not taking any narcotic analgesics
- Have regained sufficient power to push the brakes hard if required
