
Mr. Rabi Solaiman
FRACS, FAOrthA, MBBS
Orthopaedic Surgeon
Tel: (03) 9803 8066
Anterior Cruciate Ligament Reconstruction
INTRODUCTION
ACL is one of the major stabilising ligaments of the knee. It prevents abnormal movement of tibia (shin bone) and femur (thigh bone). This abnormal movement is referred to as instability. Patients’ symptoms may vary from subtle awareness to constant instability (knee giving way). ACL rupture is the most common ligamentous injury of the knee which may require surgery.
WHAT CAUSES ACL RUPTURE?
Most ACL injuries are sports related. It typically occurs when you twist your knee. It may occur following a contact injury or simply due to landing awkwardly on one leg. In either case, the knee buckles resulting in fall to the ground. There may be a pop sound as the ligament ruptures. It is usually accompanied by sudden onset of pain and swelling. Occasionally the pain may be severe enough to require attending an emergency department.
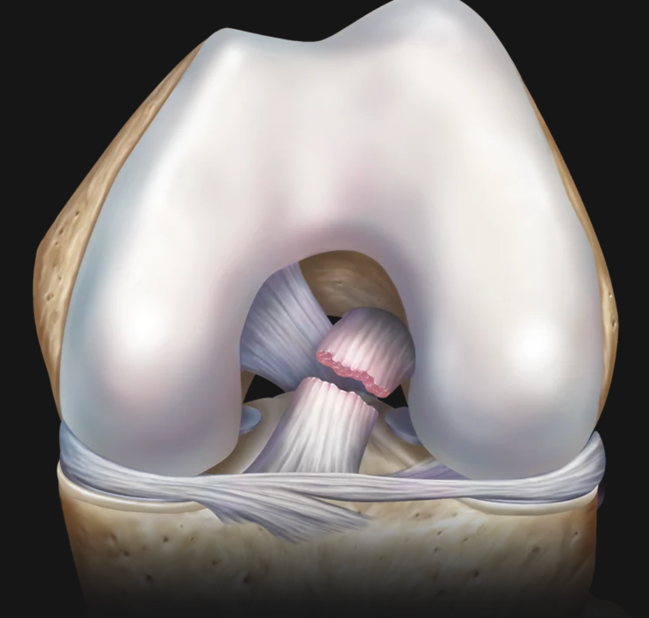
Ruptured ACL

Reconstructed ACL
HOW DO YOU MAKE THE DIAGNOSIS?
A thorough history and examination is usually sufficient to make the diagnosis. An MRI scan confirms the diagnosis. It also helps identify other structural damage prior to your surgery. In rare cases, the diagnosis can only be confirmed under general anaesthesia during surgery.
ACL rupture may occur in isolation or in combination with injuries to some of other structures in the knee. A meniscal (cartilage) tear is a common association with acute ACL rupture.
WHAT IS ACL RECONSTRUCTION AND DO I NEED IT?
ACL reconstruction involves removing the ruptured ligament and replacing it with a new graft through keyhole surgery (arthroscopic procedure). Leaving this condition untreated may lead to instability symptoms. Your knee may give way when participating in contact sports. It may even affect your daily function or work if your occupation involves pivoting the knee joint.
Constant abnormal movement due to deficient ACL may cause irreparable damage to the joint surface and menisci (cartilage). The goal of surgery is to restore the function of your knee and avoid instability symptoms. It will also protect your knee from long term damage.
BEFORE SURGERY
It is crucial that you reduce the swelling and regain your range of motion prior to surgery. Performing the surgery early while your knee is swollen with limited range is associated with risk of developing stiffness. Your physiotherapist can guide you in achieving maximum strength and range of motion prior to your procedure.
You may also be advised to cease certain medications such as aspirin or any other blood thinners. You should try to avoid getting skin cuts and scratches prior to your surgery date. These are a risk factors for increased risk of infection.
DAY OF SURGERY
Dr Solaiman will see you prior to your procedure. You will also meet the anaesthetist and the assistant. Your surgery will be under general anaesthetic. ACL Reconstruction is performed arthroscopically using 3 small incisions. The graft is obtained through an approximately 3cm incision if hamstrings are harvested. The incision for patella tendon and quadriceps tendon grafts are slightly longer.
During the procedure, Mr Solaiman will examine your knee while you are relaxed under anaesthetic. This helps determine the degree of your knee instability. He will then harvest a graft from your leg, most commonly the hamstrings. The internal structures of the knee are then examined thoroughly with an arthroscope (small camera). Tunnels are drilled in the femur (thigh bone) and tibia (shin bone). The prepared graft is passed through small holes and secured with anchors or screws. Stability of the knee is examined prior to closing the wound. Below is the link for a cartoon demonstration of an ACL reconstruction using Arthrex Graft Link.
GRAFT OPTIONS
An autograft (your own tissue) is the preferred option for ACL reconstruction. Hamstrings and Patella tendon are the two most commonly used grafts in ACL reconstruction. Quadriceps tendon has recently gained popularity in athletes returning to high-risk sports and revision surgery. In some exceptional cases, a transplant tissue (allograft or donated tissue) may be used. Although there is still no consistent consensus among surgeons as to which graft is best, most of the long-term studies have demonstrated excellent outcome with all the of autografts mentioned above. Dr Solaiman will discuss these options with you during your consultation and decide which one is best for you.
LATERAL EXTRA ARTICULAR TENODESIS (LEAT)
In some cases, where patients are at higher risk of re-rupture, an extra procedure using a separate incision may be necessary. LEAT acts as a check rein and provides extra stability. Dr Solaiman will inform you prior to surgery whether you are a candidate for the LEAT procedure.
POST SURGERY
Most patients stay in the hospital overnight. You will be able to put weight on your operated leg straight way. The physiotherapist on the ward ensures that you are mobilizing safely using crutches before you are discharged home.
Rehabilitation post ACL reconstruction is protracted. You need to see your physiotherapist on regular basis and repeat the exercises at home.
RETURN TO SPORTING ACTIVITIES
You should avoid open chain exercises for the first 3 months following surgery. You may be able to commence jogging in straight line 6 months following your ACL reconstruction providing your physiotherapist is happy with your progress. Return to pivoting activities is generally allowed about nine months from the date of surgery. It is crucial to speak to your physiotherapist regarding exercises that will help minimise the risk of re-rupture before returning to sporting activities.
Wound Care/Sutures/Dressings
Please note: It is important to keep your dressing dry at all times.
Risks
Although ACL reconstruction is a successful surgery, it does carry some risks including but not limited to infection, bleeding, blood clot, post operative pain, and graft rupture.
Individual patient’s risk profile varies based on their age and associated injuries. A history of previous blood clots increases the risk of blood clot while diabetes increases the risk of infection compared to normal population. Your risk will be assessed by Dr Solaiman and managed accordingly. Every effort will be made by the treating team to minimize your risks. If you have any concerns regarding any specific risks, please discuss it with your Dr Solaiman.
DVT Prevention
The risk of symptomatic DVT and Pulmonary Embolism (blood clot in the lung) is less than 1% following total joint replacement surgery. Studies have shown that a combination of three modalities that reduce the risk of DVT/PE include:
Early Mobilization
Foot Pump or Calf Compressors
Blood thinners
You will be given a blood thinner in addition to a mechanical device such as foot pump following surgery. You will also be encouraged to mobilize with the help of our physiotherapist as soon as possible.
Follow Up Appointment
An appointment will be made for you to see Mr Solaiman in the rooms at two weeks if you are discharged home.
